Gynaecology has been hit particularly hard by the pandemic. Millions of people are waiting for non-cancer care, while those suspected of having a gynaecological cancer are waiting far too long for a diagnosis.
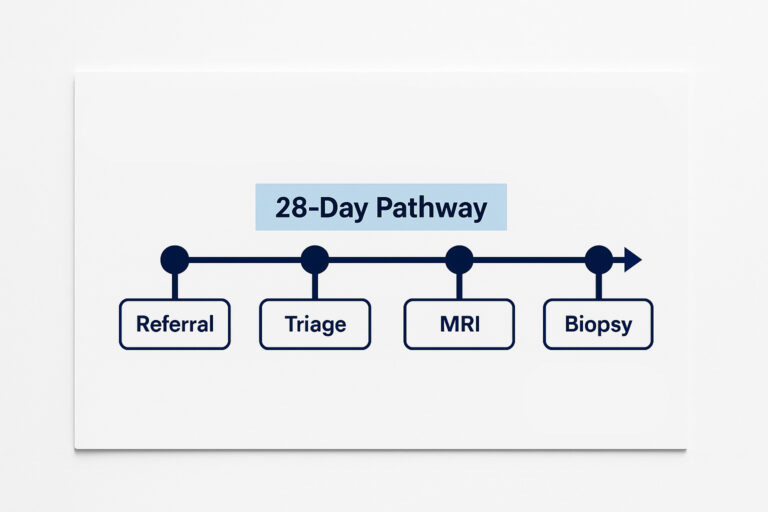
Hospitals aim to diagnose 75% of patients with suspected cancer within 28 days of referral from a GP. But the latest figures show just 67% of gynaecology patients in England have an answer within that timeframe. Many patients experienced longer waits of up to 62 days — distressing delays that can leave women anxious and uncertain for prolonged periods of time.
Patients are also waiting longer than they should for cancer treatment. The NHS says 95% of patients should begin treatment within 31 days of their diagnosis, but just 92% of gynaecology patients actually do. Long delays for diagnosis and treatment can result in worse outcomes, as the longer patients wait, the more likely their disease is to spread.
The Royal College of Gynaecologists has called on the government to commit to more funding for gynaecology services, including the training of specialists needed to deliver this care. But with the training pipeline long, it will take time for any investment in training to bear fruit.
In the meantime, independent providers are supporting NHS organisations to boost their capacity in gynaecology and help work through backlogs that can become overwhelming. SAH Diagnostics’ expert multidisciplinary teams offer tailored insourcing solutions, including end-to-end pathways, where we manage and provide care at every step of a patient’s pathway.
One trust using our gynaecology services said: “[SAH Diagnostics has] been engaged and supportive, flexing what they deliver to support what we needed. They have shown great professionalism in working across the sites with the different specialisms. They always have an eye on providing value for money particularly in procuring equipment and consumables.
“They were solution focused and willing to go the extra mile to ensure patient safety, engagement and satisfaction.”
Post-menopausal bleeding and endometrial cancer
Our post-menopausal bleeding pathway is built on national and regional guidance and the best available evidence for gynaecological care. This means we can slot easily into existing organisations, expanding their capacity while minimising variability.
In most cases, PMB will have a benign cause, like atrophic vaginitis, uterine fibroids or polyps on the womb lining or the cervix. Although they are not life-threatening, these conditions can cause significant morbidity and need to be diagnosed and treated promptly.
Sometimes, PMB will signify cancer. It’s considered a red flag for endometrial cancer, which affects the lining of the womb. One in ten women aged 60 or younger referred for their PMB will discover they have endometrial cancer, rising to 13% of women aged over 60. In some cases, PMB may indicate cervical cancer.
It’s critical that people with PMB are seen as quickly as possible, because the further womb cancer progresses, the less survivable it becomes1. When womb cancer is discovered in the earliest stage, 9 out of 10 patients will survive five years or longer. If it has spread locally in the pelvis (stage three) the five-year survival rate falls to 50%. If it spreads to other parts of the body, that rate falls to just 15%.
First steps
When a patient reports PMB to their GP, their diagnosis journey usually starts with a transvaginal ultrasound to find assess the thickness of the lining of their womb (endometrium). If this is less than 4mm, cancer is usually considered an unlikely explanation, and the patient may be treated conservatively with the potential for further investigation if other causes prove difficult to diagnose.
It’s possible causes like polyps, fibroids and other structural abnormalities will be discovered at this point. These may require minor surgical procedures.
Sometimes, clinicians will suspect malignancy on the basis of a woman’s TVUS results. If they have a thicker endometrium or polyps with risk factors such as obesity, diabetes, or hormone replacement therapy use, patients will be referred urgently for further investigations, such as a hysteroscopy or a biopsy. They may also be referred if their symptoms don’t improve or get worse.
Urgent referrals
Hysteroscopy is a specialist imaging procedure normally performed in an outpatient clinic or a day unit. It should be performed within 14 days of an urgent referral so that a patient gets a diagnosis as quickly as possible.
During the procedure, clinicians use a thin, lighted tube to look closely at the inside of the patient’s womb. They may also take samples of tissue from the womb for histological analysis. When a polyp is present, these are usually removed if possible. A sample may be taken for biopsy if they’re too large to take out.
Patients are asked in advance how they would like to receive their results. Normal results are usually sent to a patient by post. Abnormal results may be shared by telephone or clinic appointment.
Diagnosis and monitoring
When a patient is diagnosed with cancer, they may then have an MRI or CT scan, as well as tests for the levels of urea and electrolyes in their blood. Their multidisciplinary team will put together a treatment plan as soon as possible after a diagnosis, even if extra imaging tests have not yet been performed.
The nature of that plan and the appointments that come with it will depend on each patient’s particular needs. But monitoring and follow-up are provided accordingly.
SAH Diagnostic’s structured clinical pathway ensures women are assessed, diagnosed and treated in as timely a manner as possible. Our specialist staff are well-versed in national and regional PMB guidelines and will work according to best practice. Gynaecological investigations and diagnoses can be distressing for patients, so we do everything we can to ensure the best experience possible. That means providing efficient care that offers answers quickly, while making sure we treat patients with respect, care and sensitivity.
If your staff are finding it hard to meet demand for gynaecology, get in touch to find out how we can support your organisation and get your patients seen as quickly as possible.